‘Superbug River’
Croatia's biggest river puts pharma pollution under the microscope.
27 April 2020
Originally published
29 January 2020
Source
Warnings of deadly superbugs in Croatia’s biggest river raise serious questions about antibiotic pollution from drug production. Why have authorities failed to act?
From a dirt road on the north bank of the Sava river, the scene is bucolic: lush foliage, a pebble beach, sky on the water. Then you see the concrete drain, half-hidden under ivy. The air reeks of sewage. Brown foam clots in the shallows.
For microbiologist Nikolina Udiković Kolić, what is most worrying about this spot 15 kilometres upstream from the Croatian capital, Zagreb, is not what you can see and smell. It is what she found lurking in sediment around the drain — microscopic and possibly deadly. “I felt like I was doing some kind of police work,” she said, recalling the hours crouched in the mud by Croatia’s largest river, scooping sludge into sample bottles, during a year of fieldwork in 2016.
Udiković Kolić, head of the Laboratory for Environmental Microbiology and Biotechnology at the state-run Ruđer Bošković Institute in Zagreb, documented alarming levels of two common antibiotics: azithromycin and erythromycin. Worse, her team showed that the antibiotics were causing bacteria in the sediment to develop antimicrobial resistance, or AMR. In plain terms, the sludge had become a cradle of superbugs — microbes immune to the drugs designed to destroy them.
Scientists have long warned of the rise of superbugs as a dire threat to human health. “Antimicrobial resistance is one of the most concerning issues we have, similar to climate change,” said Johan Bengtsson-Palme, an AMR expert at Sweden’s University of Gothenburg. “It’s one of those things that could totally change the course of humanity in the next hundred years.”
“Antimicrobial resistance is one of the most concerning issues we have, similar to climate change. It’s one of those things that could totally change the course of humanity in the next hundred years.”
It is no secret that the world’s rivers are awash with antibiotics, sloshed into waterways as hospital effluents or flushed from our bodies into urban sewage systems. But scientists are still getting to grips with the genetic processes that spawn superbugs, and the Ruđer Bošković Institute research helped fill in some gaps. It also raised an unsettling question. Readings by Udiković Kolić and her team revealed antibiotic levels 1,000 times higher than you would expect to see from run-of-the-mill contamination. Such concentrations could only be the by-product of pharmaceutical production, the scientists concluded.
The only possible culprit: a factory in the nearby village of Savski Marof owned by Pliva, Croatia’s biggest drugmaker. Referred to in Udiković Kolić’s research as “Company 1”, Pliva has a well-documented history of polluting local waterways. It is also the only company in Croatia licensed to manufacture the active substance of azithromycin, using erythromycin as a base ingredient, according to the Agency for Medicinal Products and Medical Devices (HALMED), the state body that oversees drugmakers. The Ruđer Bošković Institute’s research was one of the first studies to link superbugs with waste from pharmaceutical manufacture in rivers in supposedly eco-conscious Europe. Pliva, owned by Israeli pharmaceutical giant Teva Pharmaceutical Industries, says independent tests show its wastewater is safe.
Authorities in Croatia appear willing to take the company at its word. Rather than jumping on Udiković Kolić ’s research as a cause for urgent enquiry, they have done little to try to recreate her results or probe the extent of AMR in the Sava. Nor do they have to. Despite international hand-wringing over the threat of superbugs, no Croatian or EU laws regulate levels of antibiotics permissible in the environment.

A concrete sewage drain discharges wastewater into the Sava river, 15 kilometres upstream from Zagreb. It was around this drain that researchers from the Ruđer Bošković Institute found alarmingly high levels of antibiotics in the water and sediment, as well as so-called superbugs. Photo: © Vedrana Simičević
Experts say such a lackadaisical approach is out of kilter with the severity of the superbug threat. “Such high concentrations [as found in Udiković Kolić’s research] clearly select for [cause] antimicrobial resistance,” said Joakim Larsson, a professor at the University of Gothenburg’s Institute of Biomedicine and a pioneer in the field. “If we pollute the environment with very high levels of antibiotics, we risk promoting the emergence of new forms of resistance in pathogens.”
A losing battle
As AMR makes antibiotics less effective, hospitals are increasingly losing the fight against infections such as pneumonia, tuberculosis, blood poisoning, gonorrhoea and foodborne diseases. Some 33,000 people in the European Union and European Economic Area die every year due to superbug infections, according to a November 2018 study by the European Centre for Disease Prevention and Control.
Scientists say the misuse of antibiotics is the leading cause of AMR, with microbes morphing into superbugs in our bodies as we needlessly pop pills to treat viral infections, for example. But evidence is mounting that antibiotic contamination of the environment is also lighting the AMR fuse. When antibiotics end up in waterways via human or animal waste, concentrations remain relatively low — typically less than one microgram per liter (μg/L). These levels are dwarfed by antibiotic concentrations from poorly treated discharge from the drug industry, studies conducted in Asia over the past decade show.
Larsson’s team at the University of Gothenburg showed in 2007 that antibiotic concentrations in effluents from around 90 manufacturing units in the Indian industrial city of Patancheru surpassed those found in the blood of a person actually taking the drug. Levels of the antibiotic ciprofloxacin were a million times higher than usually found in treated urban sewage. If you scooped up all the ciprofloxacin flowing into Patancheru waterways in a single day, you would have enough medicine to treat 44,000 people.
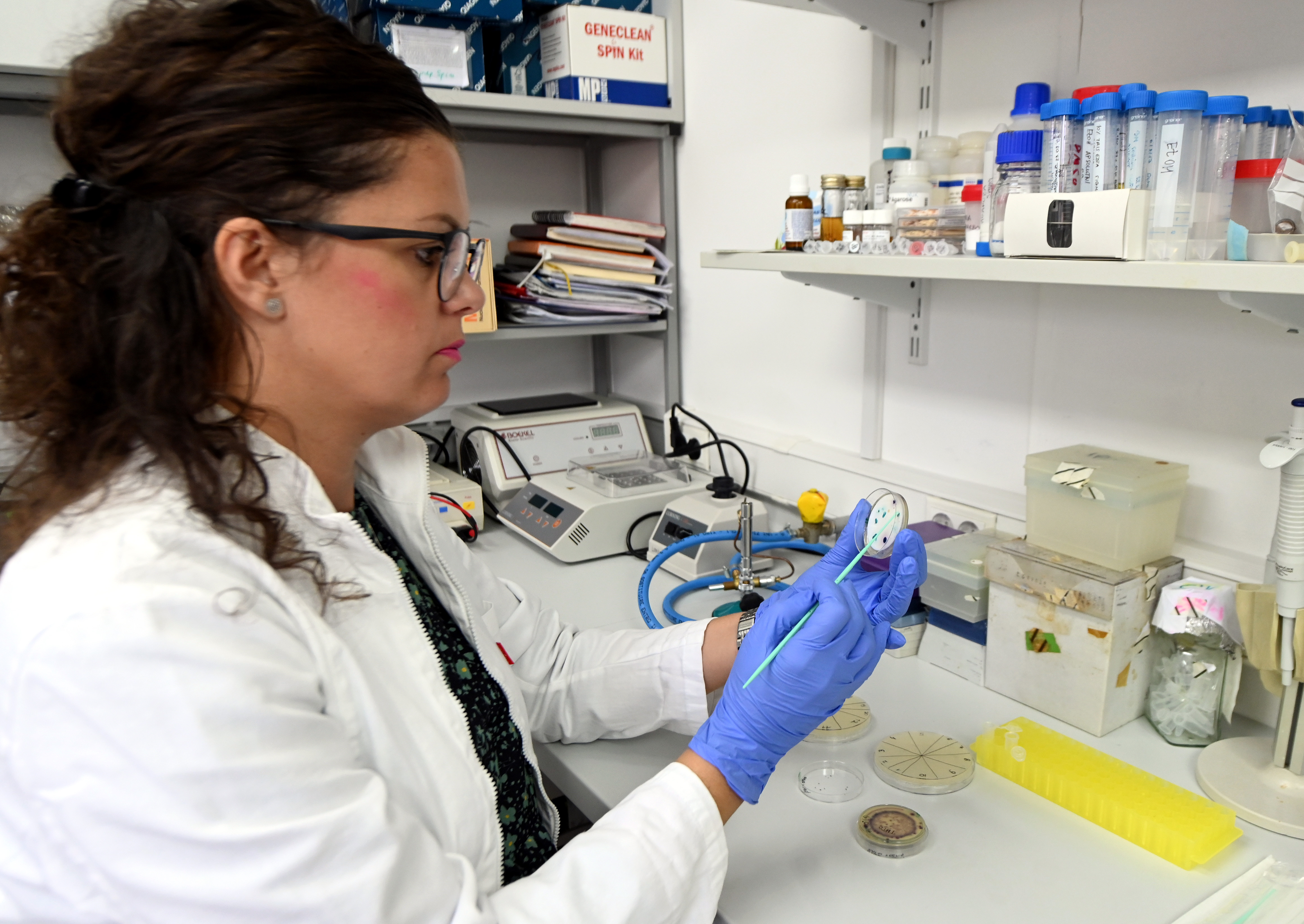
Microbiologist Nikolina Udiković Kolić works in her laboratory at the Ruđer Bošković Institute in Zagreb. Photo: © Denis Lovrović
Scientists later found similarly high concentrations in waterways in China, South Korea and Pakistan, countries known for lax environmental controls. Asked about Udiković Kolić’s research in Croatia, Larsson said it was “of very good quality”. “And yes, it shows that major pollution from drug production does occur in Europe as well,” he said.
No accident
Udiković Kolić, a 41-year-old former Fulbright scholar with a shock of frizzy hair, never set out to go to war with big pharma in 2016. Buzzing with ideas from her recent post-doctorate degree at Yale University, where she specialised in a methodology known as functional metagenomics, she was keen to explore possible links between antibiotics in the environment and antibiotic-resistant genes. Her choice of spot to hunt for contamination was no accident. Colleagues at Ruđer Bošković Institute had already detected high concentrations of azithromycin and erythromycin in the area during research conducted between 2006 and 2008.
At the time, Pliva and two other companies in Savski Marof were embroiled in a pollution scandal after years of dumping wastewater into streams including the Gorjak, a creek running into the Sava nicknamed “the Smelly” by irate locals. The other firms were French-owned yeastmaker Kvasac and US drugmaker Hospira. Ruža Katić, an activist and former local politician from the nearby municipality of Zaprešić, recalled the long and bitter fight to force the companies to clean up the Gorjak. “It was so hard to convince local authorities and the environment ministry to use available legal regulations to stop these companies from polluting the area,” she said.
“It was so hard to convince local authorities and the environment ministry to use available legal regulations to stop these companies from polluting the area.”
Things finally started to change after the agriculture ministry filed a criminal complaint against Pliva and Kvasac in 2007. The companies began sending their wastewater to the urban sewage system in Zapresic, where they were processed at the CUP Zajarki communal treatment plant. The plant is not equipped to handle antibiotic contamination. But in 2014, Pliva invested more than 13 million euros in its own treatment facility, complete with a membrane bioreactor, the latest technology for removing active pharmaceutical ingredients from effluents.
Since then, the company says all wastewater is treated on-site before it is piped to the sewage network, retreated at CUP Zajarki and discharged into the Sava from two drains about a kilometre apart. Udiković Kolić chose one of the drains for her 2016 fieldwork. She and her team tested water and sediment throughout the year, including on weekends and holidays. If Pliva’s membrane bioreactor was doing its job, antibiotic levels should have been negligible.
But on numerous occasions in the winter and spring of 2016, her team found high concentrations of azithromycin and two macrolide antibiotic by-products of the manufacture of azithromycin. The Zaprešić municipal water and sewage utility confirmed that Pliva and Hospira are the only pharmaceutical firms that discharge wastewater into the communal wastewater system. But since Hospira has never manufactured the active substance of azithromycin — a fact confirmed by state agency HALMED — the antibiotic contamination could only have come from Pliva.
The team’s results, first published the following year in the journal Water Research, revealed levels up to 10.5 mg/L — 1,000 times higher than typically found in treated hospital and sewage effluents. And even a few kilometres downstream, concentrations were 20 times higher. Control tests upstream confirmed that the contamination could not have come from elsewhere upriver. “These findings together with high levels of organic, phosphorus and nitrate compounds detected in the effluents are indicative of unsatisfactory wastewater treatment of Company 1 and of unauthorised discharges,” the team wrote in their research.

Brown foam floats on the water near the sewage drain emptying into the Sava river. Photo: © Vedrana Simičević
Something else also caught their attention: the odd timing of the findings. “On working days like Tuesday or Thursday, concentrations were low, but samples taken on Saturday afternoons or on holidays had really high concentrations of azithromycin and by-products from its synthesis,” Udiković Kolić recalled. The timings fuelled speculation that Pliva might not be using its expensive membrane bioreactor around the clock, possibly to save on operating costs, though the company denies it.
‘Croatians are poisoning us’
More frightening than the antibiotics were the superbugs found in the sediment. Udiković Kolić’s team detected high loads of bacteria resistant to azithromycin, which as Croatia’s most popular antibiotic is used to treat everything from inner ear infections to sexually transmitted diseases. Experts say AMR is making azithromycin less effective in Croatian hospitals, with the antibiotic now failing to beat pneumococcus infection in 30 per cent of cases. The fieldwork helped explain how AMR “spreads”. “The ability of bacteria to share genes is one of the fundamental factors that makes exposure to antibiotics in the environment dangerous,” said Bengtsson-Palme of the University of Gothenburg, commenting on Udiković Kolić’s research.
“The ability of bacteria to share genes is one of the fundamental factors that makes exposure to antibiotics in the environment dangerous.”
“If you have high concentrations of antibiotics, which is the case in the study by Nikolina’s lab, sensitive species and strains of bacteria will die. The one that survives will be more resistant. “The surviving bacteria can spread resistant genes to other bacteria because they are really good at sharing genes. If they are in stressful situations, they respond by saying: ‘Hey neighbours, do you want some of my genes?’ “And if those resistant genes spread to bacteria which cause disease, that means we have a clinical problem.” Udiković Kolić and her colleagues found just such a problem.
Laboratory experiments showed that hordes of resistant genes in downstream sediment were increasingly “transferring” AMR to pathogens such as Escherichia coli, often the cause of urinary and intestinal infections. Scientists say superbugs and the genes responsible for them can spread to our bodies from rivers or lakes through ingesting water, eating fish or taking part in leisure activities like swimming.
While it is not easy to prove a direct link between superbug infections and environmental antibiotic pollution, “clinical suspected cases have come to notice”, said Christoph Lubbert, head of the Division of Infectious Diseases and Tropical Medicine at Leipzig University Hospital. And even an indirect link can be dangerous, according to Arjana Tambić Andrašević , head of the department for bacteriology and hospital infections at the University Hospital for Infectious Diseases Dr. Fran Mihaljević in Zagreb.
Tambić Andrašević gave the example of E. coli bacteria developing resistance to a class of antibiotics known as cephalosporins after coming into contact with kluyvera, a bacteria that rarely causes infections but often lurks in reservoirs of resistant genes in the environment. Higher concentrations of antibiotic have also proved damaging for the ecosystem. Udiković Kolić’s team found that contaminated effluents can induce abnormalities in zebrafish embryos, for example.
The Ruđer Bošković Institute team published its findings in four different science journals over the next three years, and the results became a reference for at least two major international studies. In 2017, mainstream media in Croatia briefly reported on the research, focusing on the issue of antibiotic pollution.

Nikolina Udiković Kolić: ‘I felt like I was doing some kind of police work.’ Photo: © Denis Lovrović
Even media in neighbouring Serbia jumped on the story, alarmed at the prospect of antibiotics flowing down a river that loops across the border before discharging into the Danube in the Serbian capital, Belgrade. “The Croatians are poisoning us,” ran one tabloid headline. Despite the media attention, Croatian authorities have yet to initiate any kind of enquiry into Udiković Kolić’s findings.
‘Independent’ monitoring
The Ruđer Bošković Institute has not tested sediment samples since 2016 and BIRN was unable to independently check antibiotic levels in the Sava today. Pliva declined BIRN’s request for an interview but said in a statement that its wastewater could not have caused the antibiotic contamination found by Udiković Kolić’s team. “We stress that Pliva regularly samples wastewater from its facility on the manufacturing site of Savski Marof and conducts continuous monitoring that shows that all prescribed parameters are within allowed limits,” it said.
“Monitoring is also regularly done by independent laboratories according to methods strictly specified by authorised institutions, and collected parameters meet all prescribed norms and are within allowed limits.” The environment ministry declined to answer questions about the Ruđer Bošković Institute’s findings or Croatia’s water-monitoring policies, referring BIRN instead to Hrvatske Vode, the state water utility, and the State Inspectorate of Croatia, a government monitoring body.
According to the inspectorate, the last general inspection of Pliva’s wastewater treatment system happened at the end of 2018, without any recorded irregularities. But when it comes to keeping tabs on antibiotic levels in the wastewater, the state institutions rely on monitoring conducted by the National Laboratory of Health, Environment and Food in Maribor, Slovenia, commissioned by Pliva itself. “There is no laboratory in Croatia authorised to analyse antibiotics,” the inspectorate said in a statement.
Experts say such reliance raises questions about the independence and true accuracy of monitoring. For one thing, testing is not conducted at random and without warning. According to the inspectorate, the Maribor laboratory takes measurements six times a year at the same two spots. The first is at a point where Pliva’s wastewater enters the communal sewage system. The second is at a point in the Gorjak stream that is no longer used by the company to discharge wastewater from its pharmaceutical production. Neither point is anywhere near where scientists from Ruđer Bošković Institute recorded high concentrations of antibiotics in 2016.
Pliva declined to share data from the Slovenian lab, though it said the results “confirm that concentrations of antibiotics are always below the border of detection”. The Maribor laboratory also declined to share the results. A spokeswoman told BIRN that since the monitoring was ordered by Pliva, the data belonged to Pliva. The State Inspectorate of Croatia did not respond to BIRN’s request for detailed results from the Maribor laboratory. “Apparently it is not sufficient that the company designs the sampling themselves and are owners of the data,” Larsson from the University of Gothenburg said ironically, when asked how Pliva’s monitoring regime squares with global best practices.

A view of Pliva’s pharmaceutical factory in the village of Savski Marof. Photo: © Vedrana Simičević
He said a better system would be to place so-called passive samplers – devices or organisms designed to catch chemical pollutants in the environment over time – in the wastewater. “Although they are not very quantitative, they can reveal if there were occasional releases during the period when they have been employed,” he said, adding that “full transparency” of the methodology for sampling and analysis was a must. “Some kind of inspections on-site seem to be needed,” Larsson concluded.
No legal limits
Beyond better monitoring, experts say the real issue is regulation since there are no legal limits on antibiotic levels in the environment — meaning drugmakers can, in theory, pollute with impunity. “The standards of quality of the water environment regarding macrolide antibiotics [including azithromycin and erythromycin] are not defined in Croatian or EU laws,” state water utility Hrvatske Vode said in a statement. Nor are there regulations on antibiotic levels in wastewater from manufacturing.
‘Unintelligent Monitoring’
Across Europe, only two antibiotics — sulfamethoxazole and sulfamethazine — are widely monitored in rivers by national authorities, according to a 2018 report by the European Commission’s Joint Research Centre.
Other antibiotics, if they are monitored at all, are only done so in a few EU countries. Croatia is one of the countries that does monitor three so-called macrolide antibiotics: azithromycin, erythromycin and clarithromycin.
Hrvatske Vode, the state water utility, says it monitors these antibiotics in line with a European Commission decision (2015/495) to create a watchlist of potentially dangerous substances in water.
But the monitoring only takes place up to four times a year in the same two locations on the Sava river. The nearest is around 10 kilometres downstream from Pliva’s factory.
In most cases, “there were no significant traces of these antibiotics in the water,” Hrvatske Vode said.
Alistair Boxall, coordinator of the largest global study of antibiotics in rivers, said it was best practice to collect samples at many different spots on a given river — from six to 20 per city.
“The problem with monitoring done by regulatory agencies is that they are still looking at only a few chemicals,” he said. “In the UK, we are spending millions on monitoring the chemicals that we actually don’t use anymore and we are ignoring everything else.”
Boxall noted that the EU’s watch list of dangerous substances only contains a few pharmaceuticals.
“There is not much intelligence in the current monitoring system,” he said. “Things could be done more thoroughly, like we did in our study, or we can use some advanced analytical methods. That will certainly tell us more about what is going on in our rivers and what we are exposed to.”
In a 2018 report by the US Centers for Disease Control and Prevention, the UK Science and Innovation Network and the Wellcome Trust, experts warn of the perils of too little information on AMR in the environment — and on the manufacturing of antibiotics in general. Not only is there little published data on volumes of active pharmaceutical ingredients produced globally each year, or even where the ingredients are produced, there are no international standards for antimicrobial limits in wastewater, they say. “Specifically, greater clarity is needed on the risk to human health in order to prioritise action,” the report says.
The first independent assessment of how drugmakers are responding to the AMR threat was conducted last year by the Access to Medicine Foundation, a Dutch non-profit that lobbies the pharmaceutical industry to do more for poor people. It showed that only eight of 30 surveyed companies set limits on antibiotics released into the environment — and none published the amounts they actually pump out. “Regulatory authorities in the EU don’t require this information to be shared,” Suzanne Wolf, director of communications at the Access to Medicine Foundation, told BIRN.
In Sweden, which leads the way in Europe in addressing the environmental causes of AMR, the government has mandated the Swedish Medical Products Agency (MPA) to lobby at the EU level for tighter controls on environmental pollution from drug making. Existing regulations cover drug quality and safety but not emissions from factories, said Kia Salin, an environmental strategist at the MPA. “The pharmaceutical industry is highly against this implementation,” Salin said. “They even said that they will check this by themselves voluntarily, but there is still evidence of high levels of pharmaceutical substances in the environment around the manufacturing sites, outside and inside Europe.”
Asked about the situation in Croatia, Salin stressed the importance of independent monitoring of emissions from drug companies. “Independence should be one of the main focuses,” she said. “For several years, we have been arguing about this, at several seminars at the international level, and nothing has changed. Industry is constantly against it.” Given the information and policy vacuum, it is left to scientists and researchers to try to get a handle on the problem.
In May, the largest global study of its kind measured antibiotic concentrations in 200 rivers in 90 countries. Alistair Boxall, an environmental scientist at the University of York who coordinated the study, told BIRN that manufacturing pollution was clearly detected in some African and Asian countries, but not so much in European rivers. Still, some European locations such as the Danube channel in Vienna had “fairly high” antibiotic levels, he said.
“We compared concentrations with the proposed safe thresholds in terms of risk for antimicrobial resistance development and there were some sites in Europe exceeding those thresholds,” he said, adding that the European data is still being analysed.
In March, the European Commission adopted a Strategic Approach to Pharmaceuticals in the Environment recommending six actions to take, including gathering better data, reducing emissions from manufacturing and improving wastewater treatment. But Wolf from the Access to Medicine Foundation said: “Unless identified actions are regulated, chances are that the problem will not be improved”. For the MPA’s Salin, the commission’s strategy was a disappointment. “It has no real proposal on how we should tackle the problem,” she said. “It’s more about how we should discuss the issue for another decade or so.”
“The pharmaceutical industry is highly against this implementation.”
The University of Gothenburg’s Bengtsson-Palme said the big frustration is that environmental pollution is the easiest part of the superbug puzzle to solve. “The environmental cause of AMR plays the smaller role, opposed to misusing antibiotics in public health and agriculture,” he said. “But releasing antibiotics into the environment for no reason other than it is a little bit less costly doesn’t have any benefit.”
In 2015, he and his colleague Larsson created a list of “border” concentrations for more than 100 antibiotics high enough to trigger antimicrobial resistance. The idea was to help regulators identify levels where antibiotic pollution becomes dangerous. “If we can’t do anything about that, I can’t imagine we’ll be able to do anything about overusing [antibiotics], where it’s not just money but human and animal life at stake,” he said.
First published on 29 January 2020 on Balkaninsight.com.
This text is protected by copyright: © Vedrana Simičević, edited by Timothy Large. If you are interested in republication, please contact the editorial team.
Copyright information on pictures, graphics and videos are noted directly at the illustrations. Cover picture: The Sava river at the Croatian capital Zagreb. Photo: © Davor Puklaveć / PIXSELL / EXPA / picturedesk.com
This article was produced as part of the Balkan Fellowship for Journalistic Excellence, supported by the ERSTE Foundation in cooperation with the Balkan Investigative Reporting Network.